Pulmonary microvascular disease in diabetes mellitus (DM) subjects detected by exercise echocardiography is not associated with reduced exercise capacity (#85)
Introduction
There is limited clinical evidence of pulmonary microvascular disease (PMD) in DM. We hypothesized that (1) a novel echocardiographic marker quantifying the pulmonary transit of agitated colloid contrast bubbles (PTAC) may identify pulmonary capillary disease; and (2) that PTAC may be associated with exercise limitation.
Methods
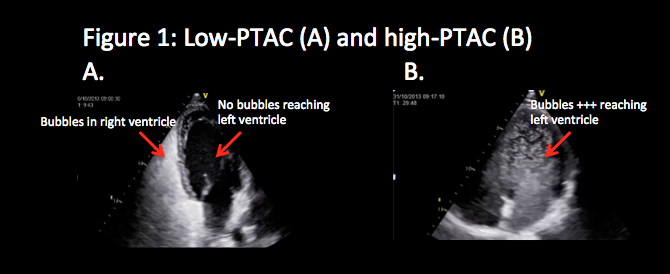
A repeated measures cross-over trial of sixty participants (40 DM and 20 age/sex-matched controls [C]) receiving sildenafil 50 mg or placebo in randomised order prior to each of two exercise tests (VO2max and exercise echocardiography) was performed. PMD was assessed by measuring the degree of PTAC traversing the pulmonary vasculature during incremental exercise, injected through a peripheral venous cannula. Bubbles reaching the left ventricle were quantified and categorised as low-PTAC or high-PTAC (see figure). Sildenafil’s effect on VO2max was observed, as were non-invasive measures of central haemodynamic parameters including cardiac output (CO) and pulmonary artery systolic pressure (PASP) to derive pulmonary vascular resistance (PVR).
Results
DM and C subjects were of similar age (44±13 vs. 43±13 years, p=0.87) and gender (70% vs. 65% male, p=0.7). Mean DM duration was 16 ± 10 years and glycaemic control was moderate (HbA1c: 7.7 ± 1.3%). At peak exercise, low-PTAC was more common in DM than C subjects (41 vs. 12.5%, χ2 P=0.041), and there was a trend to low-PTAC in DM subjects with vs. without microvascular complications (55% vs. 26.3%, Χ2 P=0.069). Sildenafil increased CO and reduced PVR in DM, without altering the frequency of low-PTAC or improving VO2max. On multiple regression, neither PTAC nor sildenafil predicted maximal VO2.
Conclusion
PTAC was lower in DM compared to C subjects thereby suggesting that PTAC may be a novel marker of PMD. However, low-PTAC was not associated with reduced exercise capacity and nor was it influenced by pulmonary vasodilator therapy.