Metformin usage in adults with type 1 diabetes in the Australian National Diabetes Information Audit and Benchmarking (ANDIAB) Initiative (#223)
Background: Insulin resistance is present in many adults with type 1 diabetes (T1D), and some physicians may consider metformin as an off-label adjunct to insulin in these patients, despite inconsistent evidence of HbA1c benefit.
Aim: To assess the prevalence of metformin usage in adults with T1D utilising the Australian National Diabetes Information Audit and Benchmarking (ANDIAB) dataset.
Methods: ANDIAB was a well-established quality program conducted by the National Association of Diabetes Centres (NADC) annually, thence biennially, from 1998-2011. It provided cross-sectional de-identified data describing the clinical status of patients attending Australian specialist diabetes services. We determined the prevalence of metformin usage in adults with T1D in the ANDIAB dataset, and compared clinical characteristics of metformin users to non-users.
Results: There were 1222 adults with T1D who had metformin data available in the ANDIAB 2009 and 2011 surveys, from 45 participating sites (metformin data not collected previously). The prevalence of metformin usage was 8.4% overall and was similar between males and females (7.9vs8.8%, p=0.13). Metformin users, compared to non-users, were older (mean 45vs41years,p=0.03) with shorter diabetes duration (mean 16vs18years,p=0.05), higher BMI (mean 32.7vs26.7kg/m2,p<0.001), higher systolic (mean 129vs123mmHg,p=0.001) and diastolic blood pressure (mean 78vs73mmHg,p<0.001), higher triglycerides (mean 1.7vs1.2mmol/L,p=0.001), lower HDL (mean 1.2vs1.5mmol/L,p<0.001) and HbA1c was similar (mean 8.7vs8.5%,p=0.29). For 624 adults with complete cardio-metabolic data, metformin users had higher rates of hypertension, dyslipidaemia, obesity and metabolic syndrome than metformin non-users (see Table).
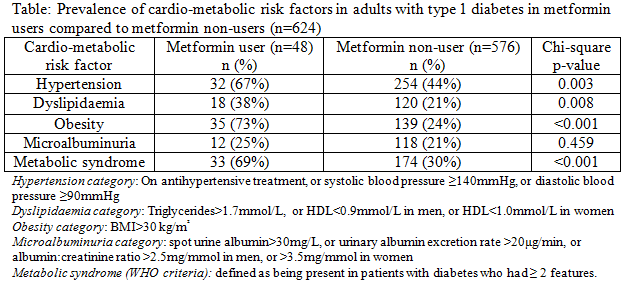
Conclusions: ANDIAB provided a valuable snapshot of clinical practices of Australian specialist diabetes services. Metformin is first-line pharmacotherapy for type 2 diabetes, but there was a significant prevalence of metformin use in adults with T1D in Australia, despite it not being TGA approved for use in T1D. The characteristics of patients taking metformin suggests that some physicians are recommending metformin in those with greater cardio-metabolic risk factors.
- Acknowledgement: With thanks to and on behalf of the NADC.